Median And Ulnar Neuropathy Assessment In Parkinsons Disease Regarding Symptom Severity And Asymmetry

Nilgul Yardimci
1Neurology Department, Minasera Aldan Hospital, Ahmet Taner Kislali Mah. 2741, Street No. 2 Cayyolu, Ankara, Turkey
2Physical Medicine and Rehabilitation Department, Medical Park Ankara Hospital, Kentkoop Mah., Kentkoop Parkici Yolu, Yenimahalle, Ankara, Turkey
3Biostatistics Department, Medicine Faculty, Hacettepe University, Hacettepe Mah., 06230 Ankara, Turkey
4Physical Medicine and Rehabilitation Department, Medicine Faculty, Turgut Ozal University, Alparslan Turkes Cad. No. 57, Emek, 06510 Ankara, Turkey
5Neurology Department, Medicine Faculty, Turgut Ozal University, Alparslan Turkes Cad. No. 57, Emek, 06510 Ankara, Turkey
6Neurology Department, Medicine Faculty, Gazi University, Emniyet, Yenimahalle, 06560 Ankara, Turkey
Abstract
1. Introduction
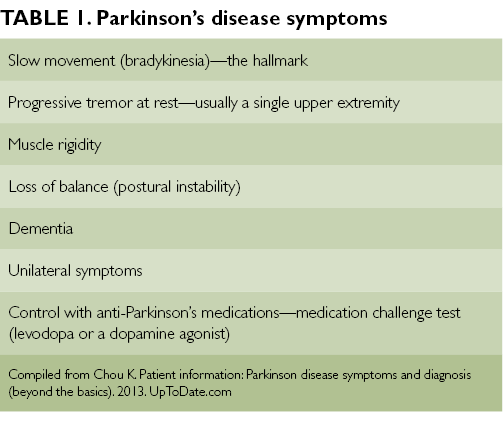
Parkinson’s disease is the second most common neurodegenerative disorder, characterised by tremor, rigidity, bradykinesia, and postural instability associated with degeneration of dopaminergic neurons in the substantia nigra pars compacta and the presence of eosinophilic intracytoplasmic inclusions .
2. Patients and Methods
2.1. Parkinson’s Disease Group
Firstly, the patients were examined for existence of any median or ulnar neuropathy according to the electrophysiologically diagnostic criteria based on control data performed in our laboratory.
2.2. Comparison Group
2.3. Electrophysiological Evaluation
2.4. Statistical Analysis
3. Results
| Variables |
Potential Pathogenic Mechanisms Of Peripheral Neuropathy In Idiopathic Parkinsons Disease Patients
The studies to date have been descriptive and associative in nature only. The precise pathogenic mechanisms for the development of peripheral neuropathy in IPD patients remain speculative. Before considering the mechanisms by which methylmalonic acid and/or homocysteine may be pathogenic, other considerations require discussion.
As mentioned, considerations for genetic influences are important. The potential implications of parkin mutations given the expression of parkin mRNA in peripheral nerve may be of importance, but only a small percentage of IPD patients with parkin mutations appear to have an axonal form of peripheral neuropathy . The relationship of concurrent peripheral neuropathy to the so called Parkinson‘s Plus forms of disease, such as with multiple system atrophy must also be considered; patients with multiple system atrophy frequently have an axonal peripheral neuropathy present . Associations such as this may suggest a neurodegenerative pathogenesis for peripheral neuropathy rather than a deficiency. Indeed, patients with greater severity and longer duration of IPD were more susceptible to development of peripheral neuropathy in our studies as well . Further studies will be required to determine if the peripheral neuropathy present in IPD patients develops in an analagous fashion to the central nervous system neurodegeneration in IPD.
Reviewperipheral Nervous System Involvement In Parkinson’s Disease: Evidence And Controversies
A variable degree of peripheral nervous system dysfunction is frequent in Parkinson’s disease patients.
- •
-
One line of evidence supports a direct damage to small nerve fibers, probably triggered by alpha synuclein deposition.
- •
-
A role of prolonged exposition to levodopa and vitamin B deficiency was also documented by independent research groups.
- •
-
In this review we provide an update on the different standpoints and discuss future directions.
Neuropathy In Parkinsons Disease Patients With Intestinal Levodopa Infusion Versus Oral Drugs
-
Affiliation Department of Neurology, Charité – University Medicine, Campus Benjamin Franklin, Berlin, Germany
-
Affiliation Department of Neurology, Charité – University Medicine, Campus Benjamin Franklin, Berlin, Germany
-
Affiliation Department of Neurology, Charité – University Medicine, Campus Benjamin Franklin, Berlin, Germany
-
Affiliation Department of Neurology, Charité – University Medicine, Campus Benjamin Franklin, Berlin, Germany
-
Affiliation Department of Neurology, St. Joseph-Hospital, Berlin-Weissensee, Germany
-
Affiliation Department of Neurology, Charité – University Medicine, Campus Benjamin Franklin, Berlin, Germany
Treatment Options For Peripheral Neuropathy In Idiopathic Parkinsons Disease Patients

In our initial case series with IPD patients identified to have peripheral neuropathy , all patients identified to have one of cobalamin deficiency, methylmalonic acid elevation, or elevated homocystine levels were prescribed monthly intramuscular injections of 1000 µg of cobalamin . This was provided via intramuscular injections and not oral therapy due to concerns of potential inadequate absorption from the gastrointestinal tract. All patients initialized on therapy were subjected to repeated clinical examinations using the Toronto Clinical Scoring System and electrophysiological evaluations at 6, 12, and 24 months after diagnosis of the peripheral neuropathy when cobalamin therapy was initiated. Repeated blood tests for cobalamin, fasting methylmalonic acid and fasting homocysteine were concurrently performed.
Is There A Natural Nerve Pain Relief Supplement For Parkinsons Patients
There is a need for additional studies on the connection between Parkinson’s and nerve pain. But initial findings show that a?natural nerve pain relief supplement?can help with pain management.
NutriNerve was designed with an innovative formula to aid patients with?nerve damage.?It is an all-natural supplement rich in vital vitamins for nerve health. Studies reveal that NutriNerve can?help the body heal?while diminishing pain and discomfort. It can become your ally in managing pain associated with Parkinson’s!
Is There A Link Between Restless Leg Syndrome And Parkinson’s Disease
Previous studies have suggested that there is a link between RLS and PD due to both conditions sharing the common feature of dysfunction in the part of the brain that produces dopamine. Another commonality between these two conditions is that they have been shown to run in the family. About half of the cases are in patients that have relatives with the disorder. Another argument for the medical linkage of these neurological disorders is that they share the same treatments – no other common disorder is treated with the same dopamine agents.
Even though earlier studies have shown a significant prevalence of RLS in patients with Parkinson’s, researchers have not been able to find a common patient demographic or Parkinson’s treatment to reliably predict the development of restless leg syndrome. Also through studies, they have found that though both conditions present dysfunction in the dopamine-producing neurons in the brain, the actual mechanisms, or how the neurons are affected, are not identical.
Earlier studies involved patients with advanced cases of Parkinson’s disease that have been taking dopamine drugs for years, which may account for the significance of RLS. The use of dopamine drugs makes it much harder to correctly diagnose restless leg syndrome. The dopamine can cause restlessness that may be confused with RLS.
How About Its Consumption In Parkinsons Disease Is It Beneficial
There is some research evidence showing that alcohol has neuroprotective function, meaning it has the ability to prevent brain cells from dying. For example, studieson animals have shown that moderate alcohol consumption may provide protection to brain cells after traumatic brain injury or stroke.
It is because of this neuroprotective effect, many think that its consumption may also benefit those with Parkinson’s disease. But this is not the case. To date, there has not been a single report published that provide evidence that alcohol consumption relieves the symptoms of Parkinson’s disease. There may be some anecdotal reports claiming that it is better for treating symptoms like tremor, but these claims are not backed by research studies. Therefore, Parkinson’s patients should be cautious and avoid excessive use of alcohol as it may further exacerbate the disease symptoms.
Parkinsons & Restless Leg Syndrome: Using Dopaminergic Medication
Because RLS is well-treated by medications that also treat PD, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in PD, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that DaTscan results are not abnormal in RLS.
Using dopaminergic medications to treat RLS however can be tricky. In some people they can lead to a phenomenon known as augmentation, in which long term use of dopaminergic medications can worsen the symptoms – making them appear earlier in the day or migrating to the upper body in addition to the legs.
Innovative Treatment Modalities For Managing Pain In Parkinson’s
Botulinum toxin
Non-dopaminergic pharmacotherapy may benefit patients with PD-related pain. Botulinum toxin , both A and B derivatives, should be considered in patients who do not respond to dopaminergic treatment optimization.1,8 Botulinum toxin injection provides localized treatment by blocking the release of acetylcholine at the neuromuscular junction.4 Local injections of BTX type A or B can be effective for persistent dystonia-related pain and central pain, based on its neuromuscular action in movement disorders plus analgesic mechanism.
A randomized, double-blind, crossover, placebo-controlled trial concluded that BTX-A in patients with PD is safe and potentially useful in treating limb pain.29 The study was conducted in patients with PD over the age of 30 years with painful limbs not responding to the optimization of anti-Parkinsonian medications. Patients were randomized to receive BTX-A injection or placebo, followed by the other treatment per the crossover design. Depending on the location of pain, patients received up to 200 units in upper limbs or up to 300 units in lower limbs. Patients experienced a significant reduction in their self-reported numerical pain score 4 weeks after the BTX-A injection , but not with placebo . There was no difference between the change with BTX-A compared to placebo . This study demonstrated that targeted BTX-A injections are safe in patients with PD.
Cannabinoids
Nerve Conduction Studies Hrus And Diagnosis Criteria Of Pnp
All patients underwent electrophysiological examination performed by a board-certified neurologist with the use of a Medtronic four channel electroneurography device . Motor studies of tibial and median nerve as well as sensory studies of sural and median nerve were done bilaterally maintaining skin temperature at 36°C and were referenced to normal values.17 Nerve HRUS examination was performed with an Affinity®70G ultrasound system with an 18-MHz linear array transducer as described previously. It was performed bilaterally at entrapment and nonentrapment sites. The entrapment sites included the median nerve , the ulnar nerve , and fibular nerve . The nonentrapment sites contained the median nerve , the ulnar nerve , and the fibular nerve . In order to avert anisotropy, the transducer was kept perpendicular to the nerves and no additional force was applied while the extremities were kept in neutral position to avoid nerve deformation. The measurement of CSA was performed at the inner border of the thin hyperechoic epineural rim by a continuous tracing technique.
The diagnosis criteria for PNP were determined by nerve conduction studies. The lower value of bilateral conduction was regarded to detect early PNP. In order to include and analyze neuropathy groups with different severity in NCS we defined three PNP subgroups based on normal values17 .
Relationship Of Vitamin B12 Status And Parkinson’s Disease
Objective/Rationale: Vitamin B12 deficiency can cause a number of neurological symptoms, including instability, neuropathy and cognitive defects. Recent studies in Parkinson’s disease patients with neuropathy have shown that B12 deficiency is common. Also, we have recently observed that B12 levels decline over the course of PD. These observations have led us to hypothesize that concurrent B12 deficiency may contribute to overall decline in some patients.
Project Description: The DATATOP study was a large study of patients with early PD conducted more than 20 years ago. As part of this study, standardized measurements of cognitive function and mobility were obtained over the course of the two-year study. Blood samples were also collected and stored. In our study, we will measure blood levels of vitamin B12 and other markers of B12 deficiency in the DATATOP subjects to determine how common B12 deficiency is in early PD and if there is a relationship between low B12 levels and early cognitive or mobility problems. Since a number of patients underwent blood testing nine or more months after study entry, we also will measure B12 levels at study completion to determine whether B12 levels decline.
The Link Between Parkinsons Disease And Toxic Chemicals

A new book calls the increasing prominence of Parkinson’s “a man-made pandemic.”
Michael Richard Clifford, a 66-year-old retired astronaut living in Cary, N.C., learned before his third spaceflight that he had Parkinson’s disease. He was only 44 and in excellent health at the time, and had no family history of this disabling neurological disorder.
What he did have was years of exposure to numerous toxic chemicals, several of which have since been shown in animal studies to cause the kind of brain damage and symptoms that afflict people with Parkinson’s.
As a youngster, Mr. Clifford said, he worked in a gas station using degreasers to clean car engines. He also worked on a farm where he used pesticides and in fields where DDT was sprayed. Then, as an aviator, he cleaned engines readying them for test flights. But at none of these jobs was he protected from exposure to hazardous chemicals that are readily inhaled or absorbed through the skin.
Now Mr. Clifford, a lifelong nonsmoker, believes that his close contact with these various substances explains why he developed Parkinson’s disease at such a young age. Several of the chemicals have strong links to Parkinson’s, and a growing body of evidence suggests that exposure to them may very well account for the dramatic rise in the diagnosis of Parkinson’s in recent decades.
Sometimes, though, the links are so strong and the evidence so compelling that there can be little doubt that one causes the other.
Neuropathy In Parkinsons Disease May Be Related To L
S. Andrew Josephson, M.D.
AccessMedicine from McGraw-Hill
Idiopathic Parkinson’s disease is a central nervous system disorder affecting the basal ganglia that is caused by death of dopamine-producing cells in the substantia nigra. Although IPD is thought classically to spare the peripheral nervous system, an association between peripheral neuropathy and IPD has been demonstrated in some of the rare genetic forms of Parkinson’s disease. A recent study aimed to examine the relationship between the more common form of IPD and PN.
The authors conducted a prospective cohort study by randomly selecting patients from a database of IPD patients at a tertiary center in Canada. Patients as well as age- and gender-matched controls underwent detailed clinical assessment, neurophysiologic testing using nerve conduction studies, and a thorough laboratory assessment for causes of neuropathy. Patients who could not tolerate these tests or who had known risk factors for PN such as diabetes were excluded.
To discern the etiology of PN in IPD patients, the authors examined a number of known causes of neuropathy, most of which were unrevealing. Although similar cobalamin levels were found in the IPD groups with and without PN, fasting homocysteine and methylmalonic acid levels were significantly higher in the IPD group with PN.
Cite this: S. Andrew Josephson. Neuropathy in Parkinson’s Disease May Be Related to L-Dopa Exposure – Medscape – Jul 15, 2010.
Tables
Parkinsons Symptoms Have Appeared What Happens Next
After the appearance of possible Parkinson’s symptoms, a neurologist will perform a comprehensive physical examination and a thorough uptake of ones medical history, including an account of medications past and present to rule out side effects that may mimic the symptoms of Parkinson’s. Scans may also be used as a diagnostic tool, such as magnetic resonance imaging of the brain to rule out a structural cause of Parkinsonism.
In addition to a diagnostic and visual exam, a neurological examination testing agility, muscle tone, gait and balance will be conducted. Results are recorded in a table known as the United Parkinson’s Disease Rating Scale . This universal scale is a vital tool in documenting the progression of the disease and establishing a timeline of symptoms. Comparisons can be made at subsequent follow-up visits.
Clinically, the diagnosis of Parkinson’s is made through the improvement of symptoms after receiving medications that stimulate or imitate the production of the neurotransmitter dopamine, such as levodopa.
Does Having Rls Increase The Risk Of Developing Pd
Since RLS affects as much as 4-10% of the US adult population, it is clear that the vast majority of those with RLS do not ever develop PD.
Despite this, it still might be the case that RLS increases the risk of subsequently developing PD. There have been many studies trying to figure this out – with conflicting results. Some studies show that there is no increased risk and others show that having RLS confers about a two-fold increased risk of developing PD over the general population.
Is There A Link Between Parkinsons And Nerve Pain
Peripheral neuropathy is a condition triggered by?nerve damage?in the peripheral nervous system. Peripheral nerves are vital for transmitting nerve signals between the central nervous system, the brain, the spinal cord, and other body areas.
It isn’t uncommon for Parkinson’s patients to experience nerve pain.?A couple of small studies show that Parkinson’s disease might be responsible for chronic pain in the hands and feet. It is believed that Parkinson’s patients are more prone to developing nerve damage.
The?symptoms common with Parkinson’s and nerve pain?include:
- Tremor
- Sexual dysfunction
- Insomnia
Even though there is no cure for Parkinson’s, many patients experience relief with physiotherapy and medication. But in most cases, there is the need for a?natural nerve pain supplement. This can diminish the discomfort and improve life quality.
Pain Management Principles In Parkinson’s Disease
Non-pharmacologic methods with a multidisciplinary pain team should be utilized to provide optimal multimodal treatment in patients with PD.4 Muscle relaxation exercises and walking regularly can improve flexibility and dampen experiences of pain associated with motor symptoms.6 Rehabilitation with a physical therapist can improve gait and balance, targeting pain caused by motor symptoms. Surgical interventions, such as deep brain stimulation or an implanted spinal cord stimulator, may be appropriate for those patients experiencing pain with PD who do not respond to pharmacologic or rehabilitation interventions.1,6,9
Optimization of treatment with levodopa and other antiparkinsonian medications should be the first pharmacological step in managing PD-related pain.6,8 Beyond this recommendation, no evidence encourages the use of specific analgesic agents in any stepwise order, making patient input and assessment of pain type critical to appropriate treatment.
Patients should be prescribed analgesics if optimization of dopaminergic agents is not effective on its own .4
Optimization of Dopaminergic Agents
Safinamide is a selective, reversible MAO-B inhibitor that reduces degradation and reuptake of dopamine to increase levels in the striatum.19 Safinamide also has non-dopaminergic properties that modulate glutamate release via inhibition of voltage-gated sodium channels. This dual mechanism may mitigate pain, especially during “off” periods.
Tackling Neuropathy Fatigue And Gi Issues In Pd
While it’s known as a movement disorder, people who live with Parkinson’s disease experience many non-movement, or non-motor, symptoms too – though not all of them are related to the disease. Peripheral neuropathy, or nervous system damage, fatigue and GI issues are common PD challenges that can also stem from other causes. Working with your doctor to identify the source of your symptoms is key to effective treatment.
This article is based on the Parkinson’s Foundation Expert Briefing series; Symptom Management: Is it PD, Medication or Aging? Exploring Non-motor Symptoms: Neuropathy, Fatigue, GI Issues presented by Ellen Walter, Nurse Practitioner, Cleveland Clinic, and Steven Swank, Clinical Pharmacist, University of Kansas Medical Center. Both organizations are Parkinson’s Foundation Centers of Excellence.
Causes of neuropathy, fatigue and impaired gastrointestinal function during the course of PD can be wide-ranging – and include everything from normal aging to medication side effects.
With any health challenge, it’s recommended to log symptoms. This can help your doctor rule out potential causes. When did symptoms start? Are there any patterns?
Most Common Causes Of Parkinsons And Neuropathy
Although specific nerve degeneration is different in Parkinson’s and Neuropathy, both diseases have the same causes across the general population. Slow bio-accumulation of toxins in the body for years, if not sufficiently flushed, results in nerve degeneration. Risk of these diseases depends on one’s overall toxic load and general level of health. There are many individual factors such as where you live, level of exposure, diet, gut health, and exercise. Here are the top causes:
Graph shows Parkinson’s deaths correlated to use of Monsanto’s Glyphosate on crops , and increased consumption of GMO corn and soy in the USA from 1985 to 2009.
Left, a healthy brain with normal dopamine activity.Right, a brain with Parkinson’s showing disrupted dopamine signaling.
Alcohol And Parkinsons Disease Is There A Link

The link between alcohol and Parkinson’s disease has remained the focus for researchers for many years. They have been trying to find out whether its consumption reduces the risk of developing Parkinson’s disease.
The first evidence in this regard came from a study conducted in Spain in 1994 that involved 74 Parkinson’s patients and 48 control subjects.
In this study, several environmental factors were investigated for their risk of developing Parkinson’s and alcohol was one of them. It was found that alcohol drinking reduced the risk of developing Parkinson’s disease in males.
Almost a decade later, similar results were reported in one information-based study involving 150 Parkinson’s patients and 150 randomly selected people from the same area. The information detail was collected by interviewing these subjects. It was found that drinking alcohol had an inverse relation with Parkinson’s disease.
But these results are contrary to the results found in studies published in the last few years. These new studies found no association between alcohol intake and risk of Parkinson’s disease. For example, a recent review study compiled results from 17 different studies concluded that there is a weak association between alcohol consumption and Parkinson’s disease. While a large prospective study published in the Journal of Movement Disorders also concluded that there is no link between alcohol intake and risk of Parkinson’s disease.
Clinical And Demographic Data Of Pnp Subgroups
Fifty PD patients were included into the analysis with a mean disease duration of 6.5 ± 5.1 years, mean levodopa dosage of 590 ± 391, and mean MDS-UPDRS III of 31.2 ± 16.6. Of the 50 patients, 31 patients fulfilled the electrodiagnostic criteria for PNP. Fourteen patients had a mild, sensory PNP, 11 patients had a moderate, sensorimotor PNP. Six patients had a severe, sensorimotor PNP.
Importantly, concerning PNP subgroups, there were no statistically significant differences between sexes, age of onset or for LED observed .
| Total PD patients | PD patients without PNP | PD patients with PNP | PD patients with mild/sensory PNP | PD patients with moderate/sensorimotor PNP | PD patients with severe/sensorimotor PNP | Healthy controls |
|---|---|---|---|---|---|---|
| Mean age at evaluation ± SD | 67.8 ± 10.4 |
The Use Of Levodopa And Peripheral Neuropathy
There are reports in the literature that levodopa use may increase the risk of peripheral neuropathy, although other studies suggest that this is not the case. There are studies that demonstrate for example, that cumulative Levodopa exposure correlates to prevalence of PN in people with PD. Other studies however, demonstrate no difference in the prevalence of PN whether the person was treated with Levodopa or not, suggesting that Levodopa treatment does not play a role in development of PN.
Another area of research that emerges from the literature is the potential role of Vitamin B12 deficiency in the development of PN in those with PD. Some studies suggest that Vitamin B12 deficiency is a more common cause of PN among those with PD than those with PN who do not have PD.
There is also research that suggests that levodopa treatment may contribute to PN through impairment of Vitamin B12 metabolism, leading to Vitamin B12 deficiency. Taking COMT inhibitors such as Entacapone may protect against this complication.
Regardless, if PN is diagnosed in anyone, whether they have PD or not, and whether they take Levodopa or not, Vitamin B12 and various other markers of Vitamin B12 metabolism should be tested. If Vitamin B12 levels are low or even low-normal, a person should take Vitamin B12 supplementation, which may help with the symptoms of PN. Other causes of PN, many of which can be checked with various blood tests, should be investigated as well.
Peripheral Neuropathy And Parkinsons Disease
A number of studies have tried to determine if PN is more common among people with PD as opposed to people without PD. PN is a relatively common condition in the general population, which makes it difficult to ascertain whether or not it is even more common among people with PD.
The available studies have varying results and are difficult to compare with each other as they:
- Include different types of populations of people with PD
- Assess peripheral neuropathy differently
- Assess for causes of peripheral neuropathy differently
A recent review looked at all the available data and determined that large fiber neuropathy was present in 16% of patients with PD, about double the prevalence of this condition in the general population. Skin biopsy-proven small fiber neuropathy was present in over 50% of people with PD, although this result was based on a small sample of patients.
General Assessment Of Peripheral Neuropathy
Peripheral neuropathy, as compared with IPD, can be due to hundreds of different etiologies , and is associated with a variety of pathological changes within a peripheral nerve. The most common causes of peripheral neuropathy are metabolic or endocrine disorders such as with diabetes mellitus, uremia, or thyroid disease, infections such as with human immunodeficiency virus or leprosy, toxic effects as with chemotherapy or alcohol excess, genetic disorders such as with Charcot-Marie-Tooth disease, amongst other causes. Another potentially underdiagnosed cause of peripheral neuropathy is a nutritional deficiency such as with insufficient vitamin B1, vitamin B6, vitamin B12, folate or thiamine . Many other causes of peripheral neuropathy occur, but between 40-50% of patients with peripheral neuropathy have no determined cause for their peripheral neuropathy, leading to its designation as an idiopathic peripheral neuropathy . Typically, idiopathic peripheral neuropathy occurs in older patients and has a slow progression over many years, but its overall clinical presentation and course of progression is similar when compared with other forms of peripheral neuropathy. There are likely a number of causes of idiopathic peripheral neuropathy, many of which may be due to neurodegenerative conditions which have not yet been determined.
Inflammatory Bowel Disease And Parkinson’s
Research has investigated the association between PD and IBD. Studies have found that there seems to be an increased risk of developing PD among people with IBD. The risk is greater among those with Crohn’s disease. A higher rate of PD is also associated with IBD patients who have hypertension , coronary artery disease, or depression.5
Characteristics Of Restless Leg Syndrome
There are certain features of RLS that make it a unique and specific disorder.
Sensory Suggested Immobilization Test
The PD+RLS group was further assessed with the sensory SIT19,20. Patients were observed in the evening, between 8?PM and 9?PM, lying down in a 45° recumbent position and instructed to move as little as possible with legs extended. Patients were asked every 10?min to indicate their perceived severity of leg discomfort, using a visual analog scale of 0–100, generating seven individual values for each participant. A mean leg discomfort score >11 was used as supportive of RLS diagnosis. This cutoff value has previously been evaluated and proposed as appropriate in the context of RLS diagnosis in PD20.
Diabetes Linked To Parkinsons Disease
Type 2 Diabetes May Raise Parkinson’s Disease Risk
March 28, 2007 — Having diabetes may increase the risk of developing Parkinson’s disease.
Finnish researchers have found that people with type 2 diabetes were more than 80% more likely to be later diagnosed with Parkinson’s disease than others.
It’s the first major prospective study to suggest that diabetes may be a risk factor of Parkinson’s disease, a progressive disease that causes muscle rigidity and tremors.
Researchers say the exact nature of the relationship between diabetes and Parkinson’s disease is unclear, but several lifestyle factors may be associated with both disorders, such as being overweight, cigarette smoking, and lack of physical activity.
“It could be hypothesized that diabetes might increase the risk of Parkinson’s disease partly through excess body weight,� writes researcher Gang Hu, MD, PhD, of the National Public Health Institute in Finland, and colleagues in Diabetes Care.
Preventing Parkinsons And Neuropathy
While reversing these diseases is considered impossible, a few brave souls have self-healed and have found a life with no symptoms whatsoever. Here’s how to prevent or reverse these diseases.
John Pepper’s instructions for “mindful walking”.
Resources:
